Peptic ulcer was long seen as one of the prime examples of a psychosomatic disease. From the 1930s to the 1980s, repressed emotions and stress were considered its main cause. “That psychic factors play a prominent role in the causation of ulcer is doubted by no one”, a 1952 JAMA review proclaimed.
The most popular theory was advanced by Franz Alexander, the father of psychosomatic medicine. He argued that ulcer patients had repressed desires to be loved and nurtured like a child but that they could not give in to these wishes because they wanted to appear strong and independent. The body, however, usually finds a way of expressing repressed emotions. In the worldview of a baby, the wish to be loved and cared for is closely associated with feeding. Therefore, Alexander advanced that unresolved dependency needs are expressed by the stomach. As peptic ulcer patients craved affection, their stomach was constantly preparing for food that would never come. This resulted in an overproduction of acid that over time resulted in the formation of an ulcer.
The common treatment of hospitalization, bed rest, and frequent feeding with milk and cream was seen as a confirmation of Alexander’s theory that peptic ulcer patients had a repressed desire to be nurtured. Scientific articles proposed psychotherapy as “the only etiologic treatment in most cases of peptic ulcer.”
Then, in the 1980s a paradigm shift occurred. Two Australian doctors discovered that peptic ulcer was caused by a germ, earning them the 2005 Nobel Prize in medicine. Ulcers, it turned out, could easily be treated by a combination of antibiotics and acid inhibitors.
In this three-part series, we will explore the dark psychosomatic history of peptic ulcer. In part I, we look at how psychosomatic explanations of peptic ulcers became so popular in the first place.

The 2005 Nobel prize
Australia in the early 1980s. Young physician Barry Marshall is staring at a cloudy broth. It is filled with mysterious gut bacteria of a 66-year-old patient with stomach problems. In one of the most iconic moments in the history of medicine, Marshall decides to drink the potion before him. It is going to make him ill but that is the intention. Marshall wants to prove that the small, spiral-shaped bacteria he has been studying, are the cause of common gut problems such as peptic ulcers.
At the time, peptic ulcer was seen as a psychosomatic illness caused by stress and repressed emotions. Marshall was one of the few physicians who challenged this dogma by reinstating the old idea that an infectious agent might be responsible. He was willing to take an unusual approach to convince his colleagues that his theory was correct. By drinking the broth, Marshall sought to fulfill the last two of Koch’s postulates. These four criteria, formulated by German physician Herman Koch at the end of the 19th century, are used to establish a causative relationship between a germ and a disease. The criteria not only require a microbe to be found in abundance in a diseased organism, but it should also be possible to isolate and culture it. Introducing it into a healthy organism should cause the same disease. Lastly, one should be able to re-isolate the microbe in the newly diseased organism.
Marshall largely succeeded in his objective.* By drinking the broth, he developed inflammation of the stomach (gastritis) and similar gut symptoms as his 66-year-old donor patient. A biopsy taken on the 10th day of the experiment revealed the presence of spiral bacteria that were in the original broth and were later named ‘Helicobacter Pylori’. Further research showed that H. pylori is indeed the main cause of peptic ulcers. In 2005 Marshall received the Nobel Prize in Medicine for this discovery, together with his colleague Robin Warren. The accompanying press release explained:“in 1982, when this bacterium was discovered by Marshall and Warren, stress and lifestyle were considered the major causes of peptic ulcer disease. It is now firmly established that Helicobacter pylori causes more than 90% of duodenal ulcers and up to 80% of gastric ulcers.”
This was quite a dramatic turnaround. A common disease that for half a century had been attributed to stress and personality features, turned out to be caused by a germ. How could medicine have gotten this so wrong for such a long time?
A disease of civilization
Peptic ulcer refers to a sore in the lining of the stomach or duodenum (the first part of the small intestine). It is characterized by symptoms such as stomach pain, bloating, and a burning sensation between meals.
In the first half of the 20th century, the incidence of peptic ulcers was rising rapidly in the western world. In England, approximately 10% of hospital beds were taken by people suffering from a gastric or duodenal ulcer. In some cases, an ulcer would bleed or perforate the mucosal wall, allowing bacteria and gastric content to leak out of the stomach. This was a life-threatening condition and some people died of it. Peptic ulcer was a serious disease. “One of the most common and feared diseases faced by gastroenterologists”, Grant Thompson recalled in his 1996 book ‘The Ulcer Story’. “Endoscopy was primitive at first, so clinical diagnosis was still paramount,” he wrote. “There certainly was no thought of doing anything with an ulcer when we saw it through the instrument.” Doctors would usually prescribe alkali to neutralize the stomach acid or perform surgery in the more severe cases but there was a lack of effective treatments.**
The sudden rise of the illness was also a mystery. Nobody knew why the prevalence of peptic ulcers was mounting so rapidly. The most instinctive explanation attributed it to the increased pace of modern life. Much like cancer, heart disease, and diabetes, peptic ulcer was seen as a disease of civilization. Life in the city was described as “ideal soil for the flowering of the ulcer temperament.”
The description of the typical peptic ulcer patient was quite similar to the Type A stereotype popularized for cardiovascular disease. It was “the doer rather than the dreamer, the active in body and mind rather than the lethargic and more contented” who developed peptic ulcer. One scientific publication stated that peptic ulcer was sometimes called “the wound stripe of civilization” as it mostly afflicted “persons who live a high-tension life, the hard driving, intelligent, alert individuals. It occurs among professional people as doctors, lawyers, musicians, theatrical folk, business executives and others who live and work under great pressure.” Peptic ulcer was seen as one of the side-effects of progress and ambition. One author, for example, remarked that “curiously enough, the desirable virtues of the modern, intensive, aggressive American, the characteristics which have been eulogized and designated as the cardinal marks of American successes, are precisely the characteristics so often reduplicated in the ulcerous type of patient.”
The stereotype of the ulcer patient as an ambitious and hardworking man was largely the result of selection bias. In hindsight, it is likely that only the well-off businessmen in the city were able to pay for X-rays or endoscopy and have their ulcers diagnosed. When all data on mortality, perforations, and hospitalization are considered, there was no socio-economic gradient for peptic ulcers in the early 20th century. After the Second World War, the illness was more common in lower than higher socio-economic classes as it still is today. The caricature of a busy executive as the type that is particularly prone to develop the illness, however, would remain central in most psychosomatic theories of peptic ulcer.
One of the major problems of psychosomatic medicine.
By the 1950s the psychogenesis of peptic ulcer had become “one of the major problems of psychosomatic medicine.” Numerous scientific articles appeared claiming that peptic ulcer resulted from stress, personality features, or repressed emotions. Over time, this was considered common knowledge. One article, for example, explained:
“Certainly based upon our present day knowledge, it can be said that most if not all ulcer patients have emotional difficulties of some severity and that emotional conflict and stress play a very important role in provoking the onset and exacerbation of most ulcers.”
Others presented these theories as established facts. A 1952 review in the Journal of the American Medical Association (JAMA) confidently proclaimed: “that psychic factors play a prominent role in the causation of ulcer is doubted by no one.”
In numerous publications, peptic ulcer patients were described as “emotionally disturbed” “obsessional” or “characteristically immature”. Most patients were males, but their female counterparts were described in a similar fashion. One article, for example, concluded:
“In this group of women with peptic ulcers there were evidences of profound personality disturbances in every instance. None of the patients could be considered emotionally healthy. Their personality façade varied from overt weakness and passivity to domination and aggressiveness.”
This begs the question of how peptic ulcers obtained such a central position in psychosomatic medicine. Today, psychosomatic research focuses on poorly understood conditions where little to no biomedical abnormalities can be demonstrated. Peptic ulcer, however, had a clear pathology that could be observed using X-ray and endoscopy. It was also a common disease that could strike anyone. So why did explanations involving disturbed emotions and personalities become so popular in the scientific literature? It seems that, next to the mysterious rise of peptic ulcers in the early 20th century, there were a couple of developments that favored a psychosomatic explanation. Most of these are fascinating stories rather than reliable data sources. In our first episode of this three-part series, we will take a closer look at these background developments.

The experiments of William Beaumont
The first story centers on William Beaumont, a surgeon in the U.S. military in the 19th century. One day a peculiar patient came to see him: Alexis St. Martin, a Canadian voyageur who had just been injured by an accidental gunshot in his stomach. Although he survived, St. Martin developed a gastric fistula, an opening inside his stomach. This allowed Beaumont to observe what was happening in the stomach in real-time. For some reason (financial difficulties seem more likely than scientific curiosity), St. Martin allowed Beaumont to perform multiple experiments with his gastric fistula. Beaumont would, for example, tie a piece of food to a string, insert it into St. Martin’s stomach and then retrieve it after a couple of hours to see how well it had been digested. It was during these experiments that Beaumont noted a link between the secretion of gastric juices and the emotional state of St. Martin. This was one of the early accounts of the famous gut-brain connection.
More than a century later, two researchers named Stewart Wolf and Harold Wolff, conducted similar experiments on a 56-year-old man named Tom. Much like St. Martin, Tom had developed a gastric fistula but instead of a gunshot, it was caused by a surgical procedure. The fistula allowed Wolf & Wolff to describe the effect of Tom’s emotions on the working of his stomach.
George Engel, the founder of the biopsychosocial model, conducted similar experiments, in the 1950s. His test subject was a baby girl with a gastric fistula named Monica. Engel was an internist rather than a psychiatrist, but studies such as these roused his interest in psychosomatic medicine.
Mid-century, the implications of these observations were considered profound. Before the discovery of H. pylori, gastric acid was believed to be the main reason why an ulcer could form. “No acid, no ulcer” was the credo. Anything that could increase the secretion of acid became a potential cause of peptic ulcers. The experiments by Beaumont, Engel, and Wolf & Wolff, even though largely anecdotal, made it plausible that mental stress and emotions were to blame.
Cushing’s ulcer
The second story features neurosurgeon Harvey Cushing. He was the foremost expert on brain surgery of his time. In 1932 Cushing published a paper on a handful of his patients in whom brain tumors were successfully removed but who subsequently died from perforated peptic ulcers. These ulcers became known as ‘Cushing’s ulcer’ but are rather uncommon today. They are the result of an acute physical injury in contrast to most cases of peptic ulcer which develop slowly over time.
Cushing believed that his cases revealed a connection between the brain and the development of peptic ulcers. In his influential 1932 paper called “Peptic ulcer and the interbrain” he speculated that overstimulation of the vagus nerve, because of stress or repressed emotions, resulted in peptic ulcer. He wrote:
“So it may easily be that highly strung persons, who incline to the form of nervous instability classified as parasympathetic (vagotonic), through emotion or repressed emotion, incidental to continued worry and anxiety and heavy responsibility, combined with other factors such as irregular meals and excessive use of tobacco, are particularly prone to have chronic digestive disturbances with hyperacidity often leading to ulcer effects….”
He added that this hypothesis did not account for all cases of peptic ulcer, but that it “offers a reasonable explanation of the majority of them.”
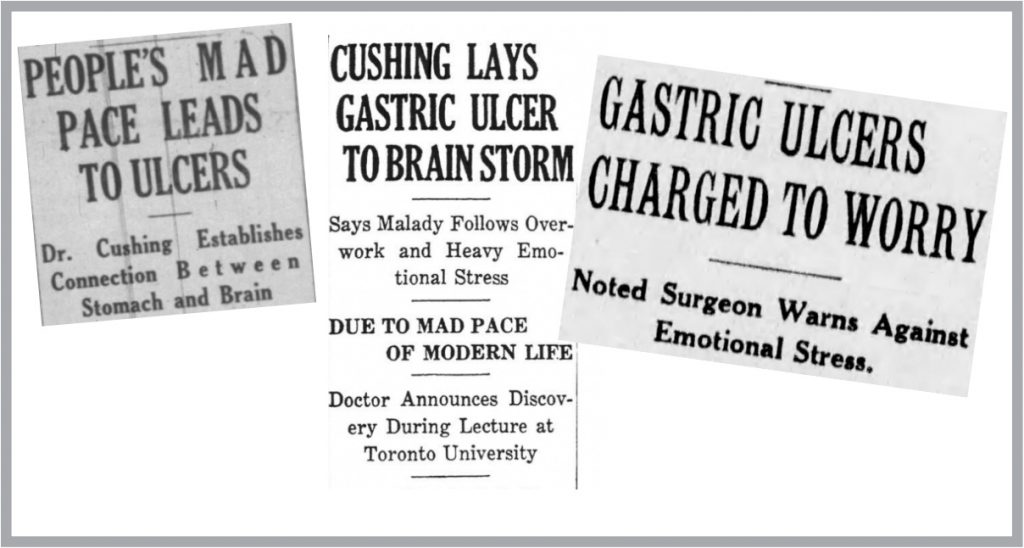
The media picked up on the story with headlines such as “Gastric ulcers charged to worry, noted surgeon warns against emotional stress” or People’s mad pace leads to ulcers, Dr. Cushing establishes connection between stomach and brain.” These newspaper reports overstated Cushing’s case and caused him a lot of worry and frustration. He felt his reputation was on the line. Ironically, Cushing subsequently developed an ulcer and attributed this to the stress and agitation this whole episode had brought him.
Cushing would die only a couple of years later but his paper on peptic ulcer would have a strong influence. The surgical procedure of cutting the vagal nerve (vagotomy) to reduce the production of acid in the stomach, would become one of the more popular treatments of peptic ulcers in the years to come.
Animal experiments and historical events
A third influence was the ethically questionable experiments conducted on lab animals.
Peptic ulcers are remarkably rare in animals despite the stresses that farm animals, for example, experience regularly. The work of Ivan Pavlov, however, showed that classical conditioning could influence the gastric function of dogs. This inspired researchers to try and induce ulcers in animals by means of psychological stress.
Unfortunately, this did not go as easily as planned and ever more extreme methods were used. Rats and monkeys were subjected to weeks of starvation with unpredictable electrical shocks when they tried to obtain food. In essence, this was a regime of torture.
Some scientists claimed to have induced ulcers with this approach and attributed these to the psychological stress in their behavioral experiments. But most of these reports were about only a handful of animals with acute lesions that differed from the chronic ulcers found in humans. The lesions were also more likely the result of starvation and electrical shock than psychological stress. Eventually, the idea of creating ulcers in animals by psychological stresses was abandoned but for many years such studies were eagerly cited to support a psychosomatic approach.
The fourth and last influence is the tales about an increase in peptic ulcers following a dramatic historical event. In the UK, for example, there were reports of an increase in perforated ulcers following the air-bombardment of London during the Second World War. These are, however, observations that did not control for factors other than psychological stress as one would do in a scientific experiment. And there were also reports during the war that did not easily fit into the stress hypothesis. In the Netherlands, for example, there was reportedly no increase in peptic ulcers during the ‘Hunger Winter’, while in Glasgow the rise in ulcer incidence preceded instead of followed the air raids. The reports of a peak in ulcer incidence following the London air raids would nonetheless be eagerly cited in the psychosomatic literature.
In part II we will take a closer look at the main psychosomatic theories of peptic ulcer, as advanced by prominent researchers such as Franz Alexander, Thomas Szasz, and George Engel.
Click here for an overview of all our articles on the dark history of psychosomatic medicine.
Notes
*Neither the donor patient nor Marshall developed a peptic ulcer. The experiment proved that helicobacter pylori could cause dyspepsia and gastritis, but more research was needed to connect this to the formation of peptic ulcers.
**Bismuth was one of many remedies used at the time. Marshall would later prove that bismuth kills Helicobacter Pylori and that it is an effective treatment for peptic ulcer. This was, however, not known at the time.
Barry Marshall is one of my heroes. I use him – and his research and methods of making himself heard – as an example. The ignorance is still with us, and applies to ME/CFS (my disease) and all the poor souls now discovering Long-covid has ruined their lives, and the doctors think it’s all in their heads – again.
You’d think they’d learn, wouldn’t you?